No matter where you live in Maine, you now have access to comprehensive cardiovascular care
Maine is a beautiful state with rocky coastlines, majestic mountains, vast forestlands, and thousands of lakes, rivers, and streams to explore. Some of the most beautiful areas of our state tend to be the most rural, away from our urban centers and our larger hospitals. Wouldn’t it be great if people could choose to live in these rural areas without having to sacrifice quality healthcare?
Northern Light Health is creating a healthcare system that is delivering high-quality care to people regardless of where they live. We are fulfilling that promise with the creation of our cardiovascular service line, which has leveraged the power of our integrated healthcare system to create comprehensive and standardized cardiovascular care that will treat people the same wherever they are — from Portland to Presque Isle and Greenville to Blue Hill.
Why is cardiovascular care so important in Maine?
Heart disease is the second leading cause of death in Maine and our population is the oldest in the country. These statistics underscore an important need that we recognized when we decided to create a systemwide cardiovascular service line in 2013. Robert Hoffmann, MD, former director, cardiovascular service line, shares, “Service lines are organized around a disease entity such as heart disease. You’re trying to develop an organized approach to treating the disease across an entire system such as inpatient care, outpatient care, homecare, emergency care, and long-term care.”
Dr. Hoffmann is a retired cardiologist who served as chairman to the working group that researched, developed, and implemented the cardiovascular service line. It was a methodical process that took two years to start showing and measuring results. “We went on the road and visited with every hospital and met clinical people and administrative people at the hospitals just to learn what they were doing, to see if they had any issues, and to tell them what we were doing,” explains Dr. Hoffmann. All that work culminated with a new organizational structure.
The cardiovascular service line is governed by a leadership council made up of cardiac and vascular physicians and cardiovascular administrators from across the system. This council is developing treatment and performance standards and quality measures and meets to review them. Those measures are updated regularly and monitored through a quality dashboard, which is a web-based application for quality reporting that is integrated into our Electronic Health Record (EHR). “What we’d like to think is that when someone has a heart problem, they can go to any one of our system hospitals or outpatient settings and receive the same quality of care wherever they are.”
When someone has a heart problem, they can go to any one of our system hospitals or outpatient settings and receive the same quality of care wherever they are.
- Robert Hoffmann, MD, former Director, Cardiovascular Service Line
Why does standardizing care matter for cardiovascular health?
Northern Light Health is an extensive healthcare system with more than 12,000 employees working in our hospitals, pharmacies, homecare agencies, emergency air and ground transport, and more.
All these organizations work together and play a role in the way we deliver cardiovascular care. We have leveraged the power of our entire system to develop a set of standards for treatment that spans the continuum of care. In addition, we have identified 14 different quality measures that we track to determine standards of care for everything from statin treatments for cardiovascular disease to readmission rates for heart failure patients.
“This is about standardizing operations, standardizing care, and standardizing quality. Is one organization doing something better than another? And if so, how do we standardize that?” stated Alan Jansujwicz, MD, medical director, Northern Light Cardiovascular Service Line.
Dr. Jansujwicz says that technology improvements such as the integration of our electronic health records (EHR) are making it much easier for Northern Light Health to compile and share data and create standardized care. That data collection can be very labor intensive, but Northern Light Health has hired consultants from Cerner, a health information technology company to assist us in installing new technology that will automate much of that data collection work.
Using this technology, we are making great strides in our treatment for congestive heart failure. We identified several areas that could be standardized including patient protocols, patient education, provider education, and transitions of care. “It’s an example of taking all our system expertise and energy, pulling it together in a group, getting some professionals from outside to help us as well, and then the goal is to push it out and improve care and standardize it across the system.”
I have never had so much attention before, and everybody worked together like a well-oiled machine. Whatever they were going to do, they told me ahead of time. They were so caring and sincere. Every person I met from Northern Light Health has been awesome.
- Nancy Lounsbury, Northern Light Mercy Hospital heart failure patient
How do you measure quality of care?
 Discharge from the hospital after surgery means you are doing well, and will continue to get better at home. Sometimes readmission to the hospital occurs.
Discharge from the hospital after surgery means you are doing well, and will continue to get better at home. Sometimes readmission to the hospital occurs.
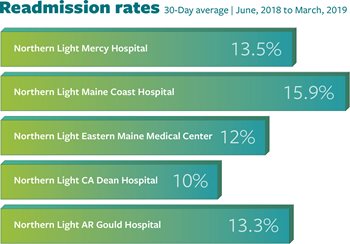
Success in the quality of your care can be measured by readmission rates. The industry goal for readmission is about 15%.
The percent of patients returning to the hospital (readmitted) at Northern Light Health is consistently low.
What is the Hub and Spokes Model of Care?
Northern Light Health is a system with many different hospitals of varying sizes, geographic locations, and capabilities from critical access hospitals to a tertiary care facility.
At the center or “hub” of our cardiovascular service line is Northern Light Eastern Maine Medical Center, a tertiary care facility that can provide the most sophisticated care for certain conditions. Our physicians and surgeons have trained at the leading cardiac centers in the world and provide the most up-to-date surgical techniques available anywhere.
With our hub and spokes model of care, we strive to broaden rural patients’ access to services by positioning a tertiary care facility as the central hub, then connecting a network of feeder or spoke facilities. Rural hospitals refer patients to the hub hospital for specialty services.
.jpg.aspx?width=400&height=320) |
We perform more than 75,000 cardiac procedures and tests each year. Northern Light EMMC houses our Structural Heart Program and our team of cardiovascular and cardiothoracic surgeons.
We also have several medium-sized hospitals, which for standard cardiology, can provide the same high level of care as Northern Light EMMC, except for specialized procedures that can only be done in a tertiary care center.
“Whether you go to Northern Light Inland Hospital, Mercy, Maine Coast, or EMMC for an atrial fibrillation visit, you’re going to get the same care,” explains Alan Jansujwicz, MD, medical director, Northern Light Cardiovascular Service Line.
Northern Light Cardiovascular Care employs two to three highly skilled cardiologists in each of these regional hub facilities that support the smaller critical access hospitals in their region. These physicians can provide the same high level of standardized care for most conditions.
Dr. Jansujwicz adds, “If your one of the small percentage of patients that need advanced care, you may go to Northern Light EMMC, but you can receive your follow up care at the hospital that is close to home.”
Whether you go to Northern Light Inland Hospital, Mercy, Maine Coast, or Eastern Maine Medical Center for an atrial fibrillation visit, you’re going to get the same great care.
- Alan Jansujwicz, MD, Medical Director, Northern Light Cardiovascular Care
What is the Structural Heart Program?
 A vital component of the cardiovascular service line is our Structural Heart Program, which is growing in popularity as it allows for minimally invasive surgery to treat many different types of structural heart disease. Structural heart diseases involve the heart’s anatomy or “structures” — valves, chambers, walls, and pockets. When the heart’s parts are not shaped correctly or damaged, blood flow can be altered, and major complications such as stroke, heart failure, or sudden cardiac arrest can follow. Some of these conditions are present from birth, while others can be acquired later in life. Until recently, the only way to treat moderate-to-severe structural heart disease was with open-chest surgery. Since the creation of our Structural Heart Program, we are proud to bring many recently approved medical advancements using minimally-invasive procedures and catheter-based interventions to the people of Maine.
A vital component of the cardiovascular service line is our Structural Heart Program, which is growing in popularity as it allows for minimally invasive surgery to treat many different types of structural heart disease. Structural heart diseases involve the heart’s anatomy or “structures” — valves, chambers, walls, and pockets. When the heart’s parts are not shaped correctly or damaged, blood flow can be altered, and major complications such as stroke, heart failure, or sudden cardiac arrest can follow. Some of these conditions are present from birth, while others can be acquired later in life. Until recently, the only way to treat moderate-to-severe structural heart disease was with open-chest surgery. Since the creation of our Structural Heart Program, we are proud to bring many recently approved medical advancements using minimally-invasive procedures and catheter-based interventions to the people of Maine.
Cardiovascular and Cardiothoracic Surgery
Operating room staff using the da Vinci Xi robot
 |
At Northern Light Cardiothoracic Surgery, our accomplished surgeons use the most advanced surgical techniques for diseases of the heart, lungs, esophagus, mediastinum, thoracic aorta, diaphragm, and chest wall.
Committed to raising quality through innovation, we use minimally invasive approaches and procedures whenever possible, including our state-of-the-art DaVinci surgical robot. Northern Light Eastern Maine Medical Center is the only hospital in Maine to offer minimally invasive esophagectomies using surgical robotic technology. Our mission is to deliver the highest quality, expert care with compassion and consideration, and our goal is to give our best to every patient, every time, and make healthcare work for our patients.
What are some of the minimally-invasive treatments offered by Northern Light Cardiovascular Care?
Watchman
This device offers an alternative to the lifelong use of warfarin for people with atrial fibrillation not caused by a heart valve problem. This permanent heart implant effectively reduces the risk of stroke — without the risk of bleeding that can come with the long-term use of warfarin, the most common blood thinner. In a clinical trial, nine out of ten people were able to stop taking warfarin just 45 days after the Watchman procedure.
MitraClip
Transcatheter mitral valve repair is catheter-based technology that uses a small clip attached to the mitral valve to treat mitral regurgitation, which is when blood leaks back into the heart through the mitral valve. MitraClip allows the mitral valve to close more completely, helping to restore normal blood flow through the heart. It’s a less invasive treatment option for patients who are not good candidates for surgery.
TAVR
Transcatheter aortic valve replacement is a catheter-based technology that inserts a replacement aortic valve while the heart is still beating. TAVR eliminates the need for an incision in the chest wall, relying instead on a minimally invasive approach. This makes the use of a heart-lung bypass machine unnecessary and provides a shorter, more comfortable recovery period when compared to a surgical aortic valve replacement.
ASD/PFO Closure
Atrial septal defect (ASD) closure and patent foramen ovale (PFO) closure are other minimally invasive catheter-based procedures that use a small, mesh, clam-shell-like device to seal abnormal communications between the chambers of the heart. ASD closure is used to seal congenital defects in the heart’s septum that can lead to pulmonary hypertension and heart failure. PFO closure, used more commonly, seals a remnant channel in the heart’s septum that in some patients can increase the risk of stroke. In recent years, there has been increasing evidence that PFO closure is more effective than blood thinners alone in preventing recurrent stroke in a younger patient with no other obvious cause.