Promises
“A promise made must be a promise kept.”
- Aristotle
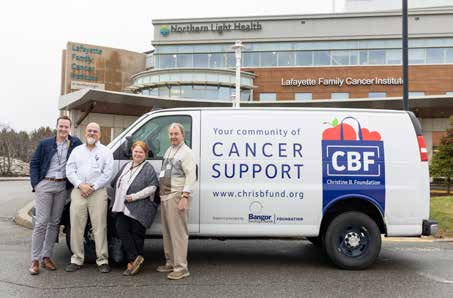
When People keep their promises to us, we feel valued, respected, and appreciated. At Northern Light Health, we understand the importance of making a promise and doing the work to keep it.
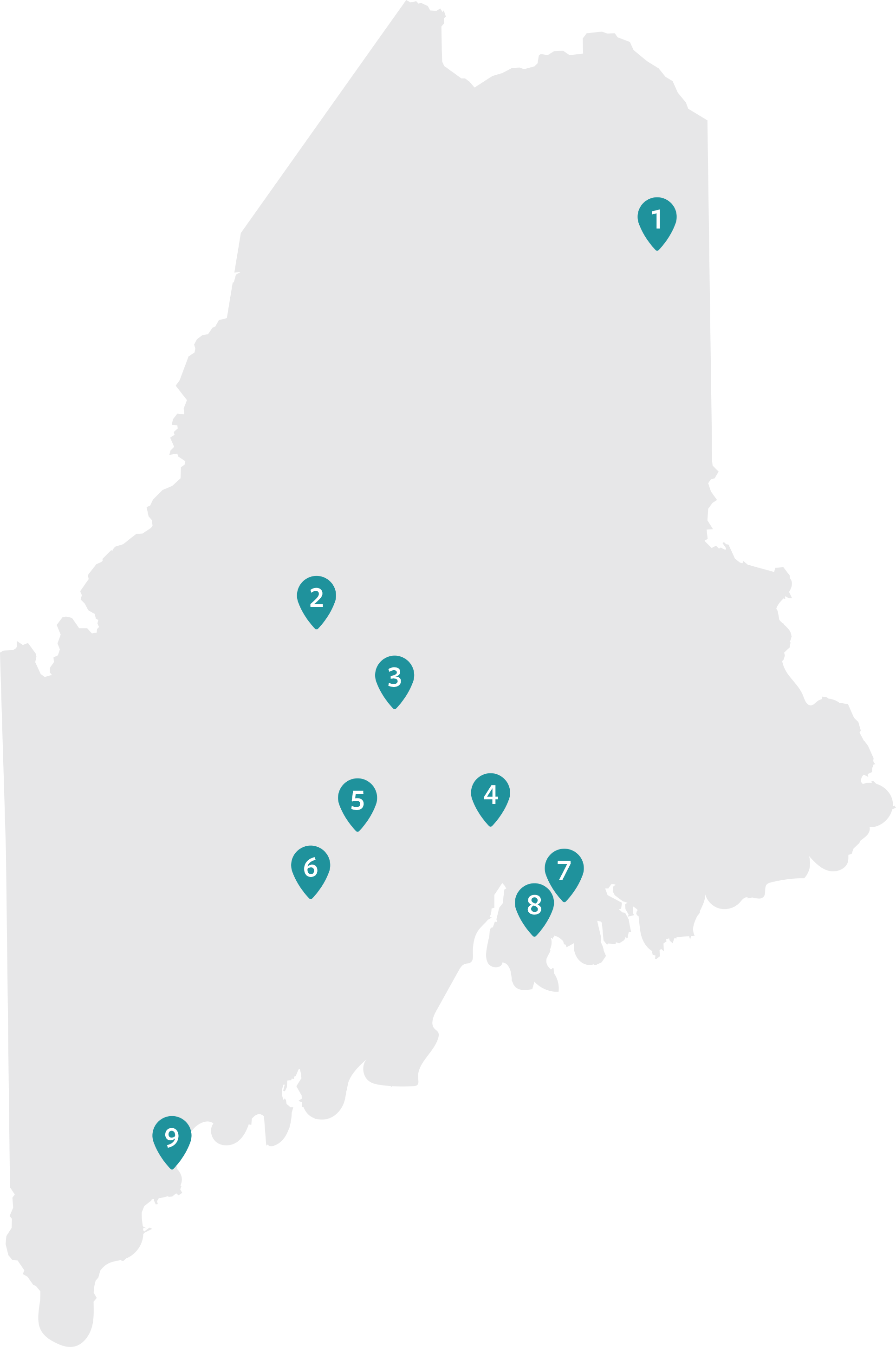
Our promise to the people and communities we serve across our great state of Maine is to make healthcare work for you. This means that we promise to get better every day by raising quality through teamwork, efficiency, and innovation. We promise to guide the way for our patients and their families, through the care experience. We live in a big, rural state, and we know access to care can be challenging for some people in our communities. So, we are committed to improving access. And last, but certainly not least, we promise to see patients as diverse individuals with their own unique needs.
In this annual report, we highlight the ways our valued employees and community partners are working together to keep our promises to the communities we serve. From helping firefighters access lung cancer studies at world-class research hospitals, to helping busy parents schedule pediatrics appointments on their own time, and using the latest in diagnostic technology to help people with congestive heart failure stay out of the hospital. We are also helping the state address a critical shortage of psychiatric inpatient beds while addressing the state's long-term community-based mental and behavioral health needs.
These stories in this report are just a few examples of the promises we work hard to keep every day. This work inspires us. We hope it inspires you too.

Tim Dentry, MBA
President & CEO
Northern Light Health

Kathy Corey
Board Chair
Northern Light Health